
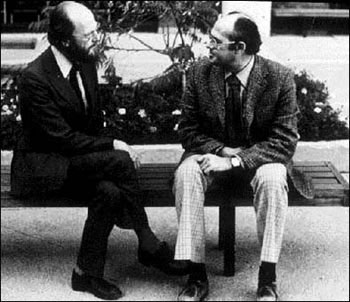
November 19 marks the 50th anniversary of the publication of the single most important scientific article in the field of pain, “Pain Mechanisms: A New Theory” (Science, 1965), co-authored by McGill’s Ronald Melzack, an experimental psychologist, and the late Patrick Wall, a sensory physiologist. The Reporter asked Dr. Jeffrey Mogil, who currently holds the E.P. Taylor Chair in Pain Studies previously held by Dr. Melzack, to explain the significance of the theory then and today, influences of the theory on his own research, and the current state of pain research and treatment.
What exactly does the Gate Control Theory propose? How was it different from the way scientists thought about pain previously?
Pain, like all sensations (although pain intriguingly is also very much an emotion, like fear; and a drive state, like hunger), is processed in the nervous system: no brain, no pain.
The first person to propose a theory about pain processing was René Descartes, who proposed that pain signals were transmitted from the affected skin (e.g., the foot touching the fire) up through the spinal cord and on to the brain, somewhere, where the perception of pain would occur. Later physiologists would discover specific pain receptors in the skin and other organs, and this came to be known as “specificity theory”.
But specificity theory couldn’t account for a number of puzzling observations about pain, such as:
- Phantom limb pain (pain in the part of space where an amputated limb used to be)
- The general failure to relieve chronic pain of surgeries in which the pain pathway up to the brain is severed
- The extremely weak relationship between the force of a stimulus and the pain it produces
- The spread of pain to areas of the body that were never injured
- The fact that rubbing a sore part of the body actually does relieve the pain somewhat, and
- the observation by Henry Beecher that soldiers in WWII often refused morphine for their grievous wounds.
As a reaction to this, other scientists proposed theories that together were classified as “pattern theory,” but these too were unsatisfactory because they ignored the existence of pain-specific receptors on nerve cells.
Melzack and Wall brilliantly combined the two into their Gate Control Theory, which proposes that both pain-specific and non-pain-specific fibers communicate with each other in the spinal cord, and depending on the relative activity of each a spinal “gate” opens, producing pain, or closes, in which case no pain signal will get to the brain and pain will not be felt. The neural circuit proposed was very specific, and was originally sketched on a cocktail napkin in a bar. A picture of that cocktail napkin can be found in the John C. Liebeskind History of Pain Collection at the UCLA library.
The paper has been cited by other scientists over 4,500 times, and continues to be cited over 150 times every year to this day. Why is it thought to be so important?
Pain scientists now believe that the spinal cord circuit proposed by Melzack and Wall is not strictly speaking accurate, but nonetheless it is considered to be the most important advance in the history of the field.
The Gate Control Theory in my mind was important for primarily two reasons. First, it gave scientists who were interested in pain something they didn’t have before, a working model to design experiments with, that would support or refute the model. They made pain research tangible for the first time. As a result, after the theory scientists started calling themselves “pain researchers;” before, they were just physiologists with an interest in pain. After 1965 pain research really started to accelerate, almost certainly because of this one paper.
Second, it really does explain in a very useful way a number of well known clinical phenomena. A good example is “counter-irritation,” the observation that pain in one part of the body can reduce pain in another part of the body. This has been known to be true for thousands of years. Growing up, every time I complained to my father that I had a headache, he would say “Come here, I’ll punch you in the arm!”
Third, the theory proposed for the first time that in addition to the spinal cord sending pain information up to the brain, the brain could send information back down to the spinal cord. In essence, the brain can tell the spinal cord, “I’m not interested in hearing about pain right now; silence!” This “descending modulation of pain” was proposed by Melzack and Wall in the absence of any evidence at all, but just a few years later evidence started to be collected that they were absolutely correct, and we now know that activation of this “Central Control” system is precisely how drugs like morphine work to kill pain.
How has the Gate Control Theory influenced your own research into pain?
I’m a behavioural pharmacologist and a geneticist, so I’ve never done much research in the spinal cord. But I’ve spent much of my career ultimately fleshing out the mechanisms and consequences of Melzack and Wall’s “Central Control” system, by which the brain can inhibit its own input about pain.
We now understand that the system evolved to be activated primarily by stress, and this phenomenon is called “stress-induced analgesia”. My laboratory has discovered many interesting things about stress-induced analgesia, in mice and more recently in humans. It’s genetically determined, with some mouse strains showing more analgesia (pain inhibition) and others less.
We even know a few of the genes. It’s sexually dimorphic in both mice and people, involving a protein called NMDAR in males, but a different protein called MC1R in females. The MC1R protein has another well-known function in that if it doesn’t work, your hair becomes red. So, yes, female redheads turn out to be more sensitive to stress-induced analgesia! We’ve shown that stress-induced analgesia can be produced by exposure to strangers, affect the results of laboratory experiments in humans, and that it can block empathy for pain.
And finally, we’ve shown that the smell of male mammals (including human men) can produce stress-induced analgesia in rats and mice. We’re currently testing to see if it can do so in humans as well. We’ve recently started doing experiments on the placebo effect, which is also thought to be produced by the activity of the “Central Control” system. All these amazing observations are utterly consistent with, and even, in a sense, predicted by, the Gate Control Theory.
What is the current status of pain research, at McGill and around the world? Are you optimistic about imminent advances in the treatment of pain?
I think it is absolutely no accident that the two most well-respected centres for pain research worldwide at the present time are the Alan Edwards Centre for Research on Pain at McGill, where Ron Melzack spent his career, and the London Pain Consortium in the U.K., where Patrick Wall spent his. Pain research as a discipline got off to a pretty slow start, probably because we’re hampered by certain limitations. Cancer researchers, for example, have the advantage of a lot of money, a relatively “simpler” disease (much of the biology happens in a single cell type), objectively measured experimental outputs (e.g., tumour size), and the enthusiastic cooperation of patients to have their tumours removed from their body for study.
By contrast, pain researchers have only about 1/100th as much money (despite the fact that chronic pain is the most prevalent human health problem, by far), a much more complicated disease (involving multiple cell types in multiple locations), no objective measure of pain, and the fact that patients are generally unhappy with requests for biopsies of their spinal cord!
Nonetheless, pain research has made great strides over the last few decades, and now pain studies are regularly accepted into the best journals in the world. Great advances are being made, using genetics, neuroimaging, and other modern approaches.
The problem is that we have done rather poorly at translating this new knowledge into fundamentally new treatments for chronic pain, which remain weakly effective and associated with problematic side effects. I think we may be turning a corner, though, with a number of interesting compounds currently in clinical trials. If and when someone comes up with a truly new and useful treatment for pain, one will be able to draw a clear line all the way back to Melzack and Wall’s 1965 paper.
