By Mark Shainblum
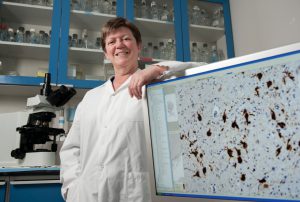
Andréa LeBlanc has found what may be a crucial key for X decoding Alzheimer’s disease (where no one was even looking).
Persistence can pay off. For the better part of a decade, Andréa LeBlanc championed an unpopular, and even controversial, theory about the root causes of Alzheimer’s disease. For most of that time, she and her team were virtually the only researchers in the world building a case against Caspase-6, an enzyme that plays a role in cell death and inflammation.
Her stance goes against the still widely held “amyloid theory,” which fingers amyloid beta (Abeta) as the fundamental cause of Alzheimer’s. Abeta forms the infamous “senile plaque” deposits, accumulations of amyloid protein in the grey matter of Alzheimer’s sufferers. LeBlanc views Abeta not so much as a criminal mastermind, but Alzheimer’s thuggish lackey, a serious demotion from cause to effect that many colleagues found hard to swallow. For the longest time, Caspase-6 wasn’t even on anyone else’s Alzheimer’s agenda.
“At the beginning, even my own students did not believe me,” LeBlanc says with a laugh. “I would get excited whenever I saw new results, and they’d just look at me as if I was crazy. “
The laughter started to die down as LeBlanc kept researching and publishing. By the time she and her colleagues had published over a dozen research papers and were demonstrating tangible and incontrovertible results, other researchers worldwide started to take notice. Some tried to replicate her results.
“We discovered that neural degeneration is totally independent of the production of Abeta,” explains LeBlanc. “This again confirmed our theory that Abeta is a consequence and not a cause of the disease. Caspase-6 is much more upstream. In fact, active Caspase-6 increases the production of Abeta in human neurons and contributes to several other cellular defects associated with Alzheimer’s disease.”
Alzheimer’s brains have extremely high levels of activated Caspase-6, while LeBlanc found virtually none in the brains of older people who did not have the disease — or in anyone under the age of 45, for that matter. She also found elevated levels of the enzyme in the brains of some older people who did not suffer from Alzheimer’s disease, but who had signs of memory impairment.
“We determined these normal people — who had active enzyme in the part of the brain thought to be first affected by Alzheimer’s disease — also had lower cognitive scores,” LeBlanc adds. “They had no clinical signs of Alzheimer’s during their lifetimes but these results indicated that they may have developed Alzheimer’s disease if they had lived longer. This makes a very strong link between Caspase-6 and Alzheimer’s disease.”
If the Caspase-6 theory is proven correct, LeBlanc sees exciting implications for the development of new diagnostic tools and therapies. Existing psychiatric methods of diagnosing Alzheimer’s are only effective once the disease has progressed past the point of no return, and there are no accepted biological or biochemical tests that can diagnose the disease in its early stages.
“Caspase-6 enzyme does not kill neurons, but it causes neurodegeneration,” she says. “The implication is that this process of neurodegeneration might be reversible. At the very least it might help us identify individuals early enough to try different therapies that could prevent the progression of the disease.”
Andréa Leblanc receives funding from the CIHR, the CFI and National Institutes of Health (U.S.).
