A team of McGill undergraduates recently won top honours at the University of Toronto’s Project X global undergraduate research competition – an annual event that challenges students around the world to use machine learning to address pressing health issues.
The group won the Clinical Practice category for its DeepVent software that uses reinforcement learning (RL) to optimize and personalize hospital ventilation treatments.
“RL models can learn from the past and can predict how the present will affect the future,” says team leader Flemming Kondrup, a U4 Honours student in Anatomy and Cell Biology. “This means that DeepVent can adapt to each patient by analyzing how they responded to previous treatments, and predict how the patient will react to future ones.”
DeepVent can adjust settings such as air pressure, the volume of air, and the concentration of oxygen in that air. Doctors usually have to manually adjust these settings as a patient’s condition evolves, a costly, complex, and often difficult task.
“We find that DeepVent is expected to not only perform similarly to physicians, but actually outperform them by 59%,” Kondrup says.
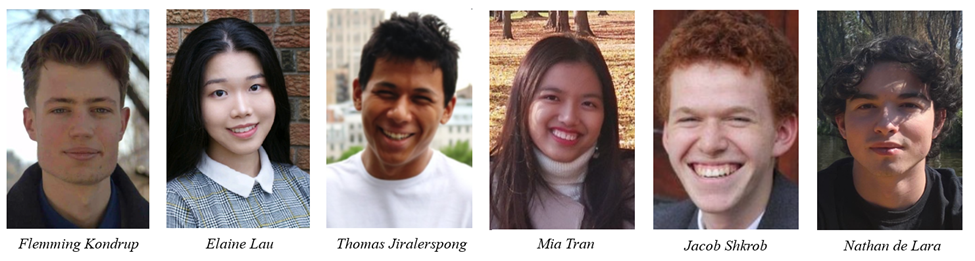
McGill’s Artificial Intelligence Society helped create Kondrup’s team last September for the competition. Kondrup’s teammates include two students in Statistics and Computer Science, Elaine Lau and Mia Tran; two students in Mathematics and Computer Science, Thomas Jiralerspong and Nathan de Lara; and Jacob Shkrob, who’s studying Probability and Statistics.
More than 150 students from 25 North American universities took part in the five-month competition, which culminated in the awards ceremony on Feb. 18-19.
Pandemic provided inspiration
Since the onset of the COVID-19 pandemic, the demand for ventilators in hospital intensive care units increased dramatically. The increased use of the devices, and the strain they place on the medical staff tasked with monitoring them constantly, provided part of the inspiration for Kondrup and his team.
“An important challenge we’re seeing during this pandemic is the pressure that is put on intensive care units and its healthcare workers,” Kondrup says. “This means that doctors or nurses don’t always have the time to check on every patient’s ventilator settings, leading to sub-optimal care. Our work would not only improve care, but also potentially automate ventilation. DeepVent could take over the role of adjusting the settings, saving essential time for doctors and nurses to focus on other tasks.”
The team has not yet come up with a plan to have DeepVent approved for hospital use, though Kondrup and his team have heard from some potential sponsors.
“The process to implement this type of technology is quite rigorous, and rightfully so,” Kondrup says. “We’re talking about the lives of patients, and that means that we need to assure high reliability and safety. This first requires the technology to get approved, and then years of clinical trials to eventually be used in clinics. We believe our work is an important stepping stone in that direction. We focus a lot on assuring safety for patients, and show that DeepVent makes recommendations within safe ranges, similar to the ones of an experienced doctor.”
The five months of hard work has landed the group a $25,000 prize.
“We haven’t yet addressed what the prize money would be used for, but supporting further works is definitely an option. I know a few people on the team are also considering going to graduate school to gain more knowledge in the field. This support could also definitely help make that possible.”
