
MUHC Geriatrics Division is busier than ever
By Fabienne Landry, MUHC Communications
Life expectancy has increased considerably over the last century. But this gift of longevity has not come without its price. Chronic illness, often combined with other health conditions, burden the lives of many of our seniors—not to mention the reduced endurance, muscle strength, vision, hearing or cognitive abilities that just naturally accompany aging. Consequently, like no other time in history, our elderly are relying heavily on our healthcare systems.
“In health facilities today, our highest patient population is the elderly,” says Dr. José A. Morais, Director of the Geriatrics Division of the McGill University Health Centre (MUHC). “And they have a physical and cognitive vulnerability, which can cause them to suffer a loss of autonomy during hospitalization. As a result, it is important for care teams to pay particular attention to these patients to prevent any avoidable deterioration in their condition.”
At the MUHC, the Geriatric Medicine Division ensures seniors are getting the best care possible with the implementation of the Specialized Approach to Senior Care (AAPA) — a ministerial directive that requires its implementation in all hospitals.
“In addition to treating the elderly with this specialized care, and training medical students and residents in this method, we encourage AAPA implementation with healthcare workers across the board so they can develop the basic skills needed to adapt their care giving to the specific requirements of the elderly and frail,” says Dr. Morais.
Limiting the risks associated with hospitalization
Sometimes hospitalization is seen as a risk for the elderly. This can be attributed to how bed rest, malnutrition, adverse effects of medication, delirium (a state of acute confusion) and an inadequate physical environment can cause complications and adverse effects in the short and long term on their autonomy and quality of life.
“One third of elderly patients who are hospitalized develop delirium during their stay in hospital,” says Dr. Morais. “Many of these cases could be avoided with care methods that are, in short, quite simple.”
The AAPA, in conjunction to existing programs of fall and bed sore prevention, helps limit these risks. Training for this approach focuses on six care dimensions that form the acronym AINÉES (elderly) in French: functional autonomy (stay active and moving); skin integrity (maintaining healthy skin); nutrition and hydration (eat well and hydrate); elimination (ensure regularity); cognitive status (stay alert and attentive); and sleep (having a proper environment for sleep).
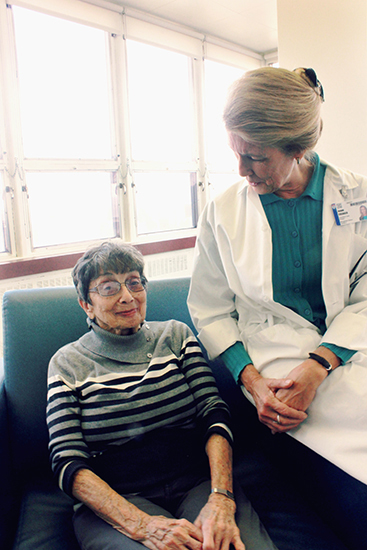
“These dimensions must be monitored and evaluated throughout the hospital stay,” says Joann Creager, MUHC clinical nurse specialist, who is responsible for teaching best practices for fellow nurses. “The goal is to reduce the risk of functional decline and delirium by paying attention to the overall health of the elderly, not only the cause of the hospitalization.”
“For example, this involves making sure that patients are moving, getting them to sit at meal time, accompanying them to the toilet instead of using a basin, ensuring that they eat and drink well, offering them an environment conducive to sleep and ensuring that noise and lighting enables them to distinguish between day and night. We must also reduce the risk of falls and ensure that the person has easy access to their dentures, glasses, a glass of water, etc.,” adds Creager.
“This year, Nursing is focussing on the development of AAPA,” says Mary Sullivan, assistant head nurse at the Geriatric Day Hospital. “In fact, this is a priority project, and not just for nurses. Orderlies, occupational therapists, physiotherapists, and all professionals, including physicians, are being sensitized to it.”
At the MUHC, when an older patient has a complex health condition, a doctor or healthcare team may also request a geriatric consultation for an overall assessment of their condition at any time.
Consultation may be conducted in both an emergency department (ED) and on the inpatient floors. It is conducted by a dyad of a geriatrician and a clinical nurse specialist. If necessary, a pharmacist who specializes in geriatric medicine may also issue recommendations, especially when patients take multiple medications (a phenomenon called polypharmacy). The simultaneous use of several drugs can have serious side effects and can sometimes lead to delirium. In the ED, the team also includes a social worker, an occupational therapist and a physiotherapist. “The geriatrician cannot cover all aspects of care alone. They must work in a team,” says Dr. Morais.
Outpatient support
Many elderly patients who have difficulty leading independent lives benefit from the outpatient services offered in most of the Montreal General Hospital of the MUHC. “Family doctors or other specialists will refer patients to us because they have developed memory problems, have lost their autonomy, or have mobility issues,” says Dr. Morais.
“Initially, nurses complete a phone screening, which includes asking the patient, and often family members, questions. After that, the patient visits the clinic for a full assessment. According to their needs, they can then be directed to our specialized services,” explains Sullivan.
“Family support is very important,” says Guylaine Bachand, a nurse specialist with 35 years of experience in Geriatrics at the MGH-MUHC. “The nurse is the bridge between the patient, the family and the rest of the team. He/she discusses the state of the patient’s health with the family and is responsible for communicating the care plan to the family doctor and CLSC staff and specialists the patient may see.”
Specialty clinics allow further assessments to be made for better targeting and treating of memory problems, pain or incapacity affecting patients. “Cognitive problems are common, with 30 per cent of people aged 85 and over suffering from memory loss. This has a great impact on their daily lives and their decision-making capability,” notes Dr. Morais.
The Geriatrics division also has a quick response system connected to clinics in order to assess the most urgent cases, and will open, at the end of November, a mobility and fall evaluation clinic.
“After the closure of a dozen geriatric beds last spring, some believed that the services of the Division would decrease,” says Dr. Morais. “The truth is our team is busier than ever ensuring our elderly patients are well cared for.”

Thank you very much for writing an informative post. Great content, I must say. Hope everybody relevant to health care industry will be helped from this content.